How Diet Shapes Your Body's Inflammatory Response
- Dr Victoria Manning

- Feb 28, 2025
- 4 min read
As a doctor with over two decades of clinical experience, I've witnessed a troubling trend: inflammatory and autoimmune diseases are rising at an alarming rate. From rheumatoid arthritis to lupus, these conditions are becoming increasingly common, especially among women. But why?
Our Bodies are on Fire: Understanding Inflammation
Inflammation is fundamentally a damage repair mechanism. When you cut yourself, inflammation helps heal the wound. When you fight an infection, inflammation battles the invaders. But what happens when this protective response never turns off?
Many of us are walking around with our "whole body on fire" due to chronic inflammation. This isn't just affecting our joints—it's a systemic issue impacting everything from cardiovascular health to brain function.
The most striking revelation? Our genetics haven't changed significantly, but our environment—particularly our diet—has transformed dramatically. This points to epigenetics: environmental influences altering how diseases manifest despite unchanging genetic code.
The Western Diet: Fuelling the Flames
The modern Western diet has shifted our omega-3 to omega-6 ratio from the natural 3:1 to an alarming 15:1 or worse. This profound imbalance creates the perfect inflammatory storm, contributing to:
- Chronic fatigue
- Persistent joint pain
- Skin conditions
- Mood disturbances
- Accelerated cellular ageing
#interesting fact -d it's not just what we're eating—it's what we're not eating. The average American consumes just 15 grams of fibre daily, while health recommendations suggest 28-35 grams. Research on the Hadza tribe in Africa, who consume up to 100 grams of fibre daily, shows virtually no chronic inflammatory diseases in their population.
The Gut-Inflammation Connection
Our gut microbiome—that complex ecosystem of bacteria living in our digestive tract—plays a pivotal role in regulating inflammation. Poor diet choices don't just add calories; they actively assault our gut barrier, leading to what scientists call "dysbiosis" and triggering systemic inflammation.
Research increasingly shows that patients with inflammatory conditions like rheumatoid arthritis have decreased gut microbiome diversity. The evidence is becoming clear: a healthy, diverse microbiome is essential for controlling inflammation.
This connection extends beyond inflammatory conditions- Remarkably, cancer researchers have discovered that patients with the most diverse gut microbiomes respond better to immunotherapy treatments. The microbiome isn't just influencing our inflammation—it's affecting how we fight cancer.
The Anti-Inflammatory Plate
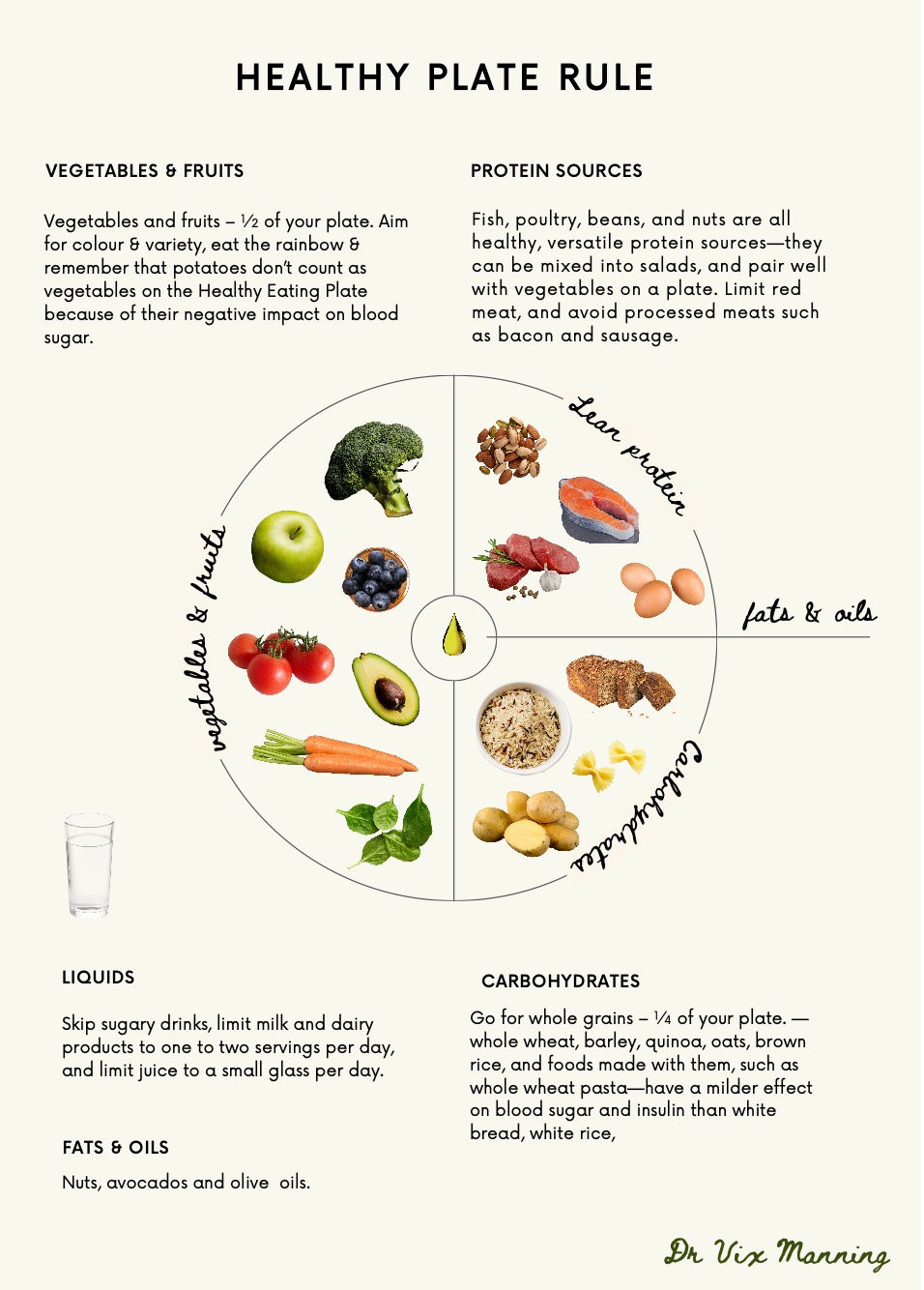
So what does an anti-inflammatory eating pattern look like? Here's a simple visual:
- Half your plate: Colourful vegetables and fruits (especially cruciferous vegetables like broccoli, kale, and cauliflower)
- Quarter of your plate: Plant proteins (beans, lentils, tofu)
- Quarter of your plate: Whole grains (quinoa, farro, bulgur, millet)
- In moderation: Animal products (aim for once weekly rather than daily)
The Blue Zones research, which studies regions where people routinely live past 100, discovered that centenarians across all zones consume roughly half to one cup of beans or lentils daily. These protein-rich legumes provide substantial fibre and nutrients that support gut health and reduce inflammation.
Omega-3 fatty acids play a crucial role in fighting inflammation. While oily fish provide these beneficial fats, concerns about heavy metals and sustainability have led many (including myself) to opt for plant-based sources like algal supplements, chia seeds, and flax seeds.
Fermented foods deserve special mention. The groundbreaking "Fe-Fi-Fo" study directly compared high-fibre diets with fermented food diets, finding that fermented foods produced more substantial anti-inflammatory effects. Including foods like kimchi, sauerkraut, and kefir can significantly improve gut health and reduce systemic inflammation.
Inflammation's Broader Impact
The National Cancer Institute has identified 13 cancers definitively associated with obesity and inflammation, including many gastrointestinal cancers and hormonally-driven cancers like breast cancer.
Research from the World Health Organisation has highlighted concerns about processed meats (like those tempting charcuterie boards with salamis and cured meats we all enjoy) and red meats, linking them to increased cancer risk. This correlates with troubling trends in colorectal cancer diagnoses in younger adults, which is why screening guidelines in the United States now recommend starting at age 45 rather than 50.
Inflammation also accelerates cardiovascular disease, diabetes, and cognitive decline. This isn't just about preventing arthritis—it's about protecting your entire body from premature ageing and disease.
Small Changes, Big Impact
Here's what I find most encouraging when working with patients: sustainable changes bring lasting results. You don't need to radically transform your diet overnight or embrace perfection. Those who gradually incorporate more anti-inflammatory foods often experience a fascinating revelation—they become more attuned to how specific foods affect their bodies.
The key is creating a sustainable approach that works for your lifestyle. Small, consistent changes deliver far greater benefits than strict regimens abandoned after a few weeks. This means those occasional treats aren't just permissible—they're an important part of a balanced relationship with food. Enjoying that piece of cake at a birthday celebration or having a cheeky glass of wine with friends can be vital for your mental wellbeing, which itself influences inflammation levels. What matters most is your overall pattern of eating, not individual indulgences
# Dr. Vix's Takeaways
Here are my key recommendations for reducing inflammation through diet:
1. Prioritise plants Aim for half your plate to consist of colourful vegetables and fruits, with cruciferous vegetables (broccoli, kale, cauliflower) taking centre stage.
2. Embrace beans and legumes: Include at least ½ cup daily of beans, lentils, or other legumes—nature's perfect anti-inflammatory protein package.
3. Focus on fibre: Target 30+ grams daily through whole foods, Remember, fibre feeds your beneficial gut bacteria.
4. Balance your omegas: Test, don't guess your omega-3:6 ratio. Consider algal-based omega-3 supplements if your levels are low.
5. Include fermented foods: Add kimchi, sauerkraut, kefir, or other fermented foods daily to support microbiome diversity.
6. Limit inflammatory triggers: Reduce ultra-processed foods, refined sugars, and saturated fats. Consider animal products as occasional additions rather than dietary staples.
7. Monitor your response: Pay attention to how different foods make your body feel, especially if you have inflammatory conditions.
The science is clear: inflammation is the common denominator in most chronic diseases, and diet is our most powerful tool for bringing the fire under control. By nourishing our gut microbiome and choosing anti-inflammatory foods, we can transform our health from the inside out.
.



Comments